Antibiotics have arguably been the single most important discovery of modern medicine and their invention has saved millions of lives.
But, to understand the current problem with antibiotics, you need to go back to Albert Alexander, a policeman working in Oxford in 1941. He had the misfortune of being scratched on the face by a rose. A bacterium, called Staphylococcus caused such a severe infection that one of his eyes had to be removed, and he became critically unwell.
Luckily for Albert, he became the first patient to be treated with Penicillin, the first commercially available antibiotic. Unluckily, not enough of the drug was available, and despite an initial improvement he succumbed to his infection.
Mass production was the key, and manufacturing was scaled in time for the Normandy invasion in 1944. And so, the global antibiotic arms race began.
Resistance is futile
Over 154 million prescriptions for antibiotics are now written each year in the USA. The problem is that 30% are unnecessary; 44% of these are written to treat patients with acute respiratory conditions which are often not caused by bacteria.
Bacteria are very clever. Resistance to drugs can be acquired by sharing mobile genetic units (called plasmids) between bacteria; this is known as “horizontal’ evolution. When resistant bugs are in the hospital where you are getting treatment, it is therefore very easy for them share resistance genes.
If you want to see what this looks like, check our this terrifying experiment. It demonstrates that bacteria can withstand a dose of antibiotic 1000 times the initial strength within 5 generations:
Antibiotics are also widely used for preventing infections in live stock, and as a result they are in our food chain and resistance be passed from food to fork as well as from person to person.
But, resistance is not a new problem. I work at St. Mary’s Hospital, London (Now Imperial College London) where Sir Alexander Fleming famously discovered Penicillin. He warned us about this problem at the time and he even noted in his Nobel acceptance speech:
But, we didn’t listen.
New drugs now cost about $2 billion to develop and it may take 10 to 20 years to bring to market. The FDA approval rate for new antibacterial drugs has also fallen from about 20 from 1980 to 1984, to less than five from 2005 to 2009. Antibiotics are cheap, and you may only use them intermittently, so there is very little incentive for drug companies to make more.
Is this the end of modern medicine?
Probably not. BUT antibiotic resistance will cause 10 million deaths globally by 2050 at a cost of £66trillion ($100trillion) to the global economy.
We are now effectively in a post-antibiotic era, where the drugs literally don’t work. This means that common infections and minor injuries can kill, and we may not be able to safely perform operations where we rely on antibiotics to prevent complications.
Which bugs should we be afraid of?
The WHO recently published a list of 12 families that pose the greatest threat to human health.
In the USA, the first case of multi drug resistant E.Coli was identified that was resistant to antibiotics colistin and carbapenems. This may have even contributed to the death of Hugh Hefner.
We have also seen the first death from a multidrug resistant Klebsiella pneumoniae, a bug that often causes of urinary tract infections. Testing at the hospital showed resistance to all 26 drugs the hospital had.
There has also been an alarming rise in the spread of multi drug resistant gonorrhoeaIs there a solution for antibiotic resistance?
Yes, but we need to act now.
This week is Antibiotic Resistance Awareness Week!
In 2016, the United Nations passed a resolution to tackle drug-resistant infections, calling for an international effort across human, animal and environmental health.
The UK government has a strategy and it wants to halve inappropriate prescribing by 2020 and to halve healthcare-associated, Gram negative bloodstream infections (GNBSI) by 2020.
New antibiotics are also coming. For example, teixobactin, was discovered in a screen of uncultured bacteria and it does not demonstrate resistance.
But the most important thing we can do now is maintain the value of existing and future antibiotics. This means:
- Only take antibiotics when you need them. So don’t ask your GP or family doctor to give you an antibiotic for your sniffles. It won’t work, and it will make the situation worse.
- If you are in contact with someone who has a bacterial infection, wash your hands and use sensible precautions to prevent spread.
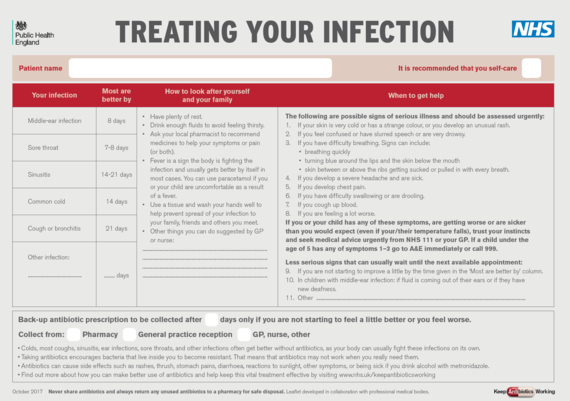
- If you do have a bacterial infection, The NHS has issued advice for this, and this can be found here:
- If you are given antibiotics, take the full course you are prescribed. This view is being challenged but for now it’s sensible.
One thing is certain. If we don’t act now, then we will go back to a time when a simple scratch from a rose thorn could be fatal.