We often talk of more than 4 in 10 cancers being preventable, through things like not smoking, cutting down on alcohol and maintaining a healthy weight.
We can say this because of years of robust evidence. This evidence shows that these and other behaviours – along with things in our environment we can’t necessarily control – can cause cancer by damaging our cells’ DNA.
But the picture of what causes cancer isn’t complete.
Enter Professor Sir Mike Stratton, director of the Wellcome Trust Sanger Institute in Cambridge, and his team from the UK, the US and the International Agency for Research on Cancer in France.
Over the last decade they’ve uncovered patterns of damage to the DNA inside cancer cells that can’t be tied to a known cause.
Now, with the £20 million they recently received through our Grand Challenge award, they aim to fill in these gaps and tie these patterns to a cause.
Their goal is to dramatically improve our understanding of what causes cancer, potentially preventing more cases in the future.
Finding the fingerprints
Everyone in the world is identifiable by their fingerprint – a unique pattern of marks that distinguishes one person from another.
But identifying patterns aren’t only found on our fingers. Our cells have them too.
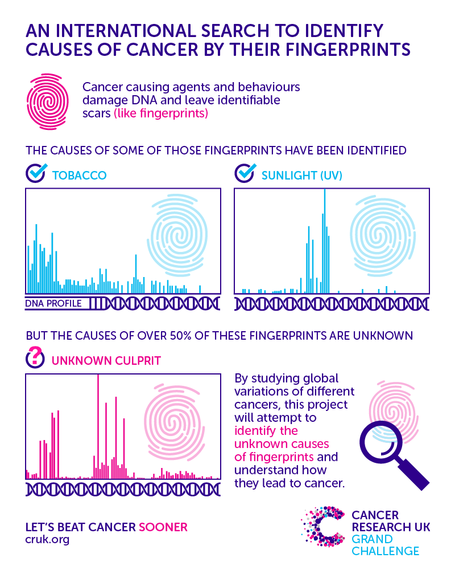
Instead of being a unique pattern of circles and whirls, these cellular ‘fingerprints’ – also called mutational ‘fingerprints’ – are made from unique patterns of genetic changes buried in our DNA.
“As cells go through life, they pick up mistakes in their DNA. And depending on the number and type of mistakes, a cell develops its own distinct mutational ‘fingerprint’,” explains Stratton.
“These ‘fingerprints’ provide clues on how a cell has lived its life, so by studying them we can not only identify what mistakes are in a cell, but also what caused them.”
Right now, scientists have uncovered around 50 mutational ‘fingerprints’ inside different cancer cells – so-called cancer-associated mutational fingerprints.
But they only know what causes around half of them.
“We know what the mutational ‘fingerprint’ associated with cancers caused by ultraviolet light and tobacco smoke look like,” says Stratton.
“And we know that in some cases there’s more than one fingerprint per cause.”
“But we’re still in the dark about what causes around 50 per cent of the mutational ‘fingerprints’ we see in cancer.”
According to Stratton there may also be other cancer-associated mutational ‘fingerprints’ yet to be discovered.
And if there are, his team aim to find them, as well as tying the remaining known ‘fingerprints’ to a cause.
High vs low – the answer is in the differences
Stratton estimates that some known cancer-associated mutational ‘fingerprints’ are caused by mistakes that happen randomly through natural cellular processes.
For the rest, he believes the causes are likely to be preventable ones associated with specific things like smoking or exposure to other cancer-causing chemicals (carcinogens).
To identify these preventable factors – and to figure out exactly how they cause cancer – Stratton and his team will study samples collected from 5,000 pancreatic, kidney, oesophageal and bowel cancer patients.
Spanning 5 continents, these samples will come from patients in countries that have either a high or low level of these cancers – something Stratton explains is central to the project.
“If we think about some of the most common types of cancer, which include the ones we’ll be studying, there are parts of the world where they are common, and other parts where they are rare.”
“For example, the number of people diagnosed with squamous cell carcinoma, one of the types of oesophageal cancer we’ll be looking at, is 100-fold higher in Iran and East Africa than in other countries.”
“But we don’t know what’s causing this massive difference.”
This isn’t the only example of one type of cancer being more common in certain parts of the world than others, something we explored in a recent series of blog posts.
For some of these differences, scientists have theories about what’s behind them. They believe there’s a cause -something our cells are exposed to- that’s responsible.
To find these unknown causes, they will read the complete DNA sequence from cancer cells in the 5,000 samples they’ll collect from patients in each continent. They will then study these DNA sequences to identify the mutational ‘fingerprint(s)’ present in each sample.
Armed with this information, the team will compare mutational ‘fingerprints’ for each of the 5 cancer types. And they’ll cross-reference this against the countries with high and low levels of each particular cancer.
By doing this, they hope to determine which ‘fingerprints’ are more common – or potentially only present – in samples taken from patients in countries with high levels of a specific cancer and which, at the same time, are less common – or even absent – in countries with low levels.
From here, the team’s challenge will be to determine what caused the mutational ‘fingerprint’ – and if it’s something that could be prevented.
To do this, they’ll study the habits, lifestyles and environments of patients who have generously donated samples to the research.
‘There’s a genuine desire and willingness from people to be involved’
Making all this global effort work, collaborating across continents, collecting patient information and samples, is something Stratton describes as an enormous logistical challenge.
That’s why the team have formed a “crucial and invaluable” collaboration with Dr Paul Brennan and others at the International Agency for Research on Cancer (IARC), which is the World Health Organisation’s cancer agency.
“At IARC, we have a large network of partners around the world whom we’ve worked with for many years looking at many different cancers,” explains Brennan.
“That puts us in a really good position to help Professor Stratton and his team achieve their goal of collecting 5,000 patient samples from across 5 continents.”
For this project, Brennan and his IARC colleagues have standardised how the participating groups around the world should collect, store and send the patient samples. This is to make sure that all of the samples are handled in the same way as much as possible.
They also clearly explain what information they need from patients about their lifestyles and habits, again to make sure the information they gather can be compared across continents, each with different health services and challenges.
But one thing that hasn’t been a huge challenge, says Brennan, is getting research partners interested in being involved in the project.
“We’re already talking to our partners in some countries, and everyone is really excited about the project. There’s a genuine desire and willingness from people to be involved,” he says.
This is in part due to the fact that IARC has a good history of working with academic hospitals and national cancer institutes across the world, and they’re a trusted UN organisation who have the means to work on a global scale.
But even more than that, he thinks people want to be involved because of the potential of the project.
“People recognise that this project, which is taking place on a massive scale, has the potential to unlock new causes of cancer. That’s something people want to be part of.”
Of mice and men
As well as all the work involving patient samples, the team will also carry out experiments in the lab with mice and lab-grown tumours (organoids) made from human cancer cells.
Stratton explains that right now, there are about 100 chemicals and exposures that scientists think might play a role in causing cancer. But they don’t know if they definitely do. And if they do, it’s not clear what mutational ‘fingerprint’ these potential causes might generate.
With their lab based experiments, his team aim to understand more.
“We’ll be doing the reverse of what we’re doing with patient samples,” Stratton explains.
“Instead of looking at the mutational ‘fingerprint’ in a cell and working out what caused it, we’re going to expose cells in the lab to certain chemicals and exposures like radiation, and see what ‘fingerprint’ it leaves behind.”
Preventing more cancers
Stratton is excited about analysing the DNA sequences and seeing the results of what the ‘fingerprints’ might hold.
But he is also keen to see “how in the future this work might help prevent more cases of cancer by identifying unknown, preventable causes of it”.
While they have theories about what these causes might be, Brennan and Stratton are clear that the answers can only come through doing this research.
“I’m absolutely sure that we’ll see surprises along the way as we analyse the data,” says Brennan. “That’s why I won’t speculate or make predictions about what we might find.”
And as Stratton explains: “This is science – there is no certainty about what we’ll find along the way. That’s what makes it exciting.”
The work Stratton and his team are doing aims to dramatically improve our understanding of what causes cancer.
If successful, it could lead to better information for people looking to reduce their risk of cancer, and also help inform government policies to reduce people’s exposure to cancer-causing agents.
Yes, it’s still a cliché, but prevention really is better than cure.
And this research could help make our ability to prevent certain cancers even more effective.
— This feed and its contents are the property of The Huffington Post UK, and use is subject to our terms. It may be used for personal consumption, but may not be distributed on a website.